Pulmonary surfactant in premature babies Idea
Home » Trend » Pulmonary surfactant in premature babies IdeaYour Pulmonary surfactant in premature babies images are available in this site. Pulmonary surfactant in premature babies are a topic that is being searched for and liked by netizens today. You can Download the Pulmonary surfactant in premature babies files here. Get all free images.
If you’re looking for pulmonary surfactant in premature babies images information connected with to the pulmonary surfactant in premature babies interest, you have pay a visit to the ideal blog. Our website frequently provides you with suggestions for viewing the maximum quality video and image content, please kindly hunt and locate more enlightening video content and graphics that fit your interests.
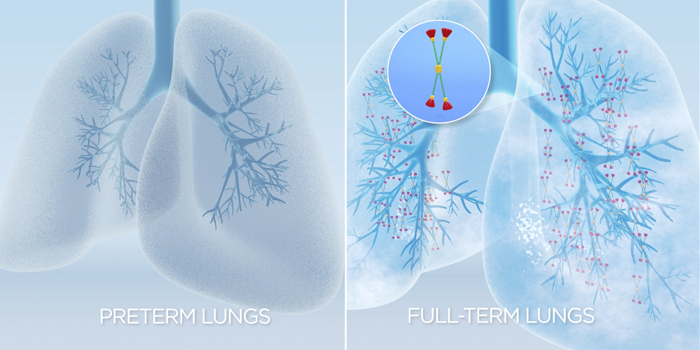
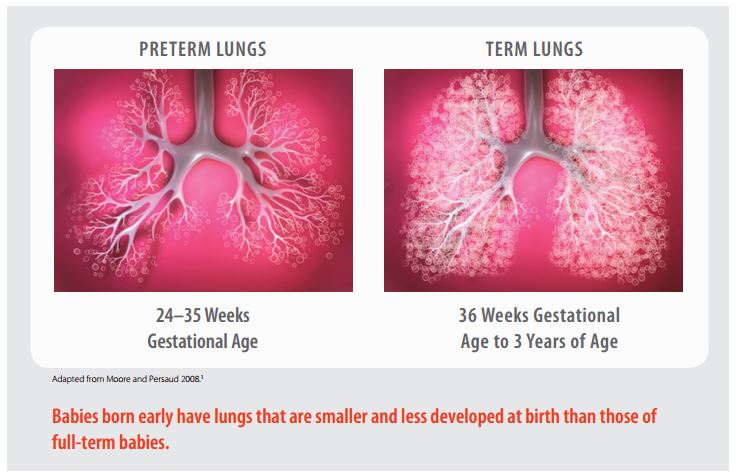
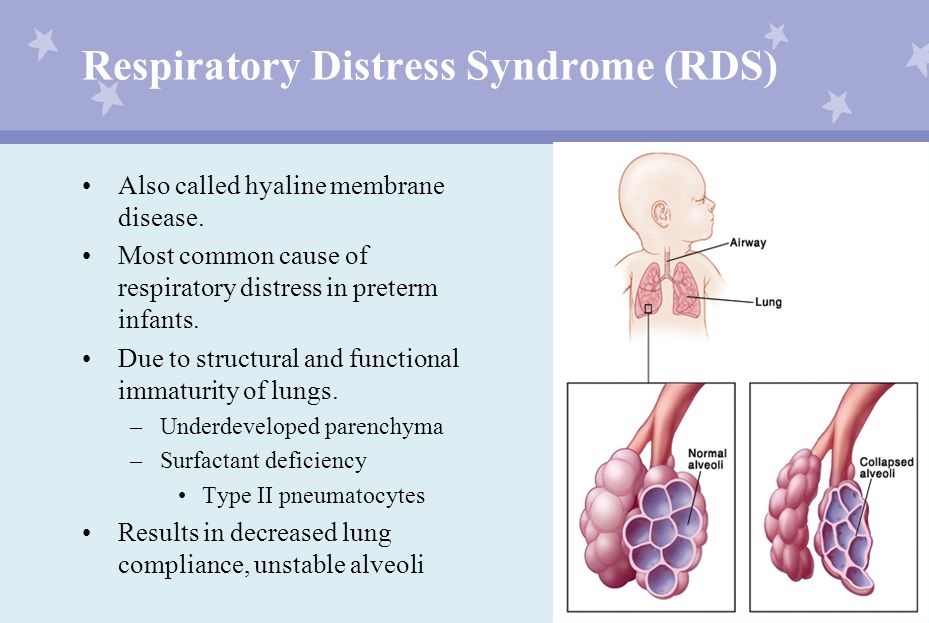
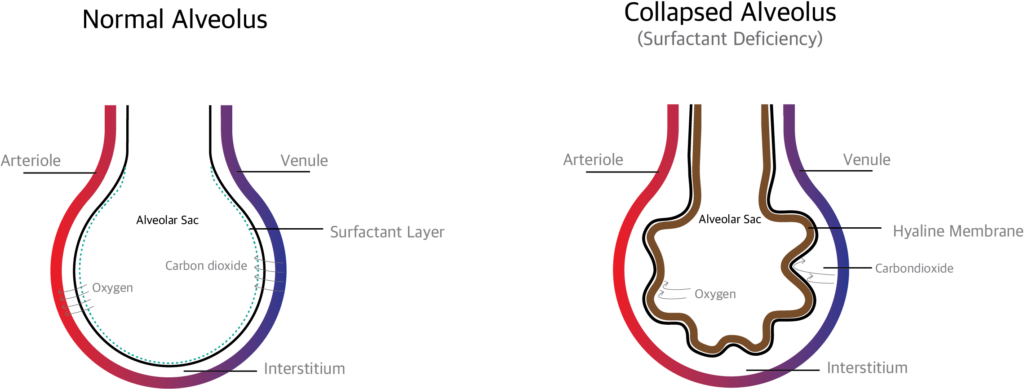
Pulmonary Surfactant In Premature Babies. 24 dying stillborn, 15 dying soon after birth and 16 dying between 2 weeks and 1 year of age with minimal lung pathology. When a premature infant whose lungs are not producing enough surfactant is born, those lungs are unable to provide the infant with enough oxygen, which results in respiratory distress syndrome. 24 dying stillborn, 15 dying soon after birth and 16 dying between 2 weeks and 1 year of age with minimal lung pathology. Similarly one may ask, how do premature babies get surfactant?
 Bronchopulmonary Dysplasia (BPD) Airway Therapeutics From
Bronchopulmonary Dysplasia (BPD) Airway Therapeutics From
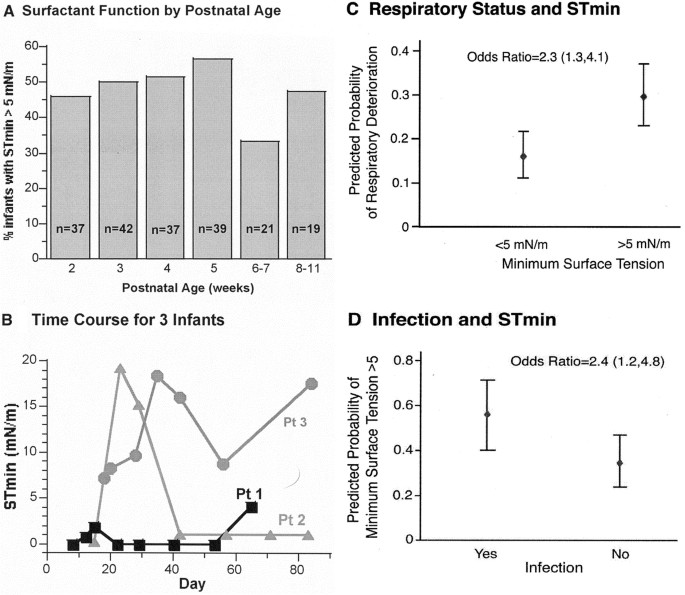
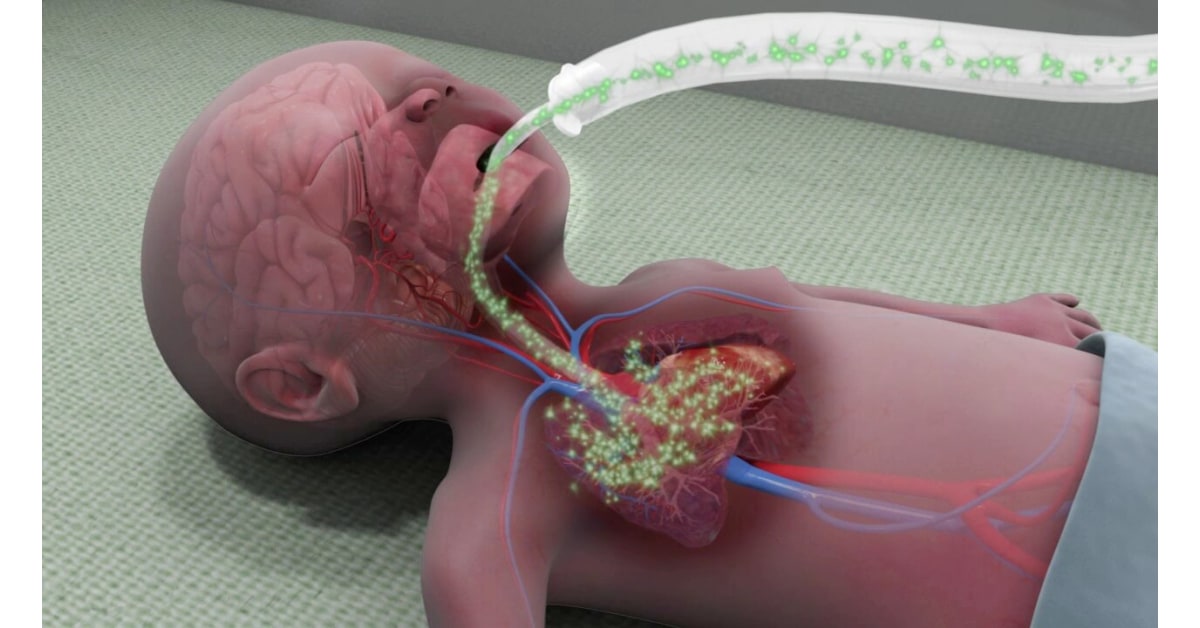
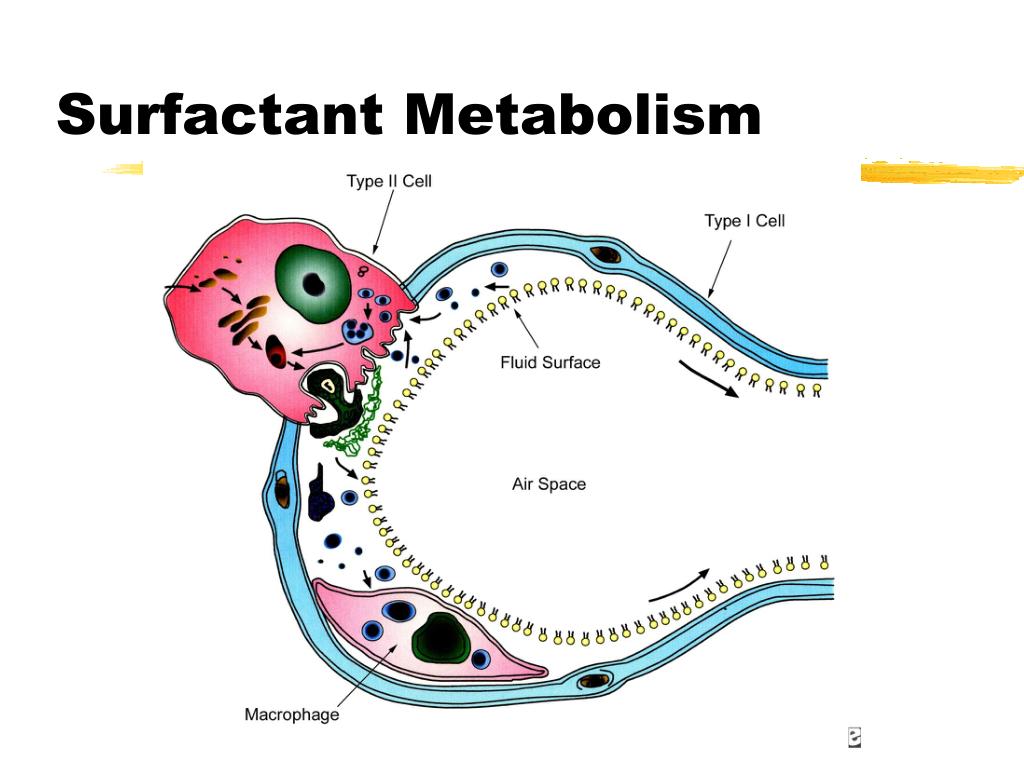
Preterm infants with respiratory distress syndrome (rds) requiring surfactant therapy have been traditionally receiving surfactant by intubation surfactant and extubation technique (insure), which comprises of tracheal intubation, surfactant administration, and extubation. Treatments that specifically target reducing surfactant inactivation would be more effective in adults than replacement lung surfactant therapies that were developed to provide premature babies with lung surfactant. According to the guardian’s choice, premature infants were grouped into treatment with pulmonary surfactant (ps) combined with nasal continuous positive airway pressure (ncpap; Synthetic surfactants have been developed and can be used for babies born prematurely (before 34 weeks) who have rds. Metabolism of surfactant is slower in newborns, especially preterm, than in adults. Its main function is to reduce the surface tension at the air/liquid interface in the lung.
Early on, during autopsies, pathologists found stillborn babies’ lungs weirdly inelastic.
24 dying stillborn, 15 dying soon after birth and 16 dying between 2 weeks and 1 year of age with minimal lung pathology. Natural surfactant is produced by the fetus before they are born and their lungs are prepared to breathe properly by about 37 week gestation. The presence of such molecules with surface activity had been suspected since the early 1900s and was finally. 24 dying stillborn, 15 dying soon after birth and 16 dying between 2 weeks and 1 year of age with minimal lung pathology. Lung surfactant was obtained by postmortem lavage from: Premature babies often require a surfactant injection to help their lungs to work.
 Source: paediatricfoam.com
Source: paediatricfoam.com
Premature babies often require a surfactant injection to help their lungs to work. 1 systematic reviews of randomized, controlled trials confirmed that surfactant administration in preterm infants with established respiratory distress syndrome (rds) reduces mortality, decreases the incidence of pulmonary air leak (pneumothoraces and. Steroids work best when they are given between 24 hours and 7 days before birth, so theyre not useful in every pregnancy. Surfactant in preterm infants introduction pulmonary surfactant is a complex mixture of phospholipids and proteins that serves to reduce alveolar surface tension. Natural surfactant is produced by the fetus before they are born and their lungs are prepared to breathe properly by about 37 week gestation.
 Source: handtohold.org
Source: handtohold.org
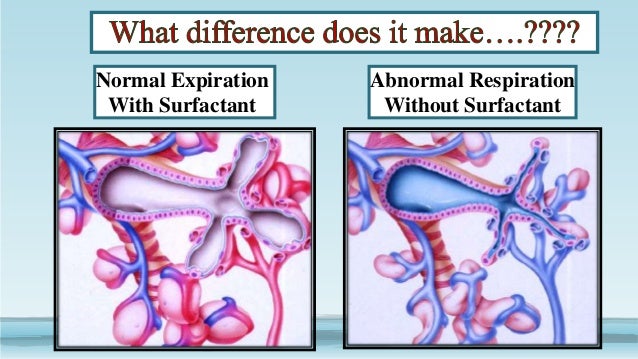
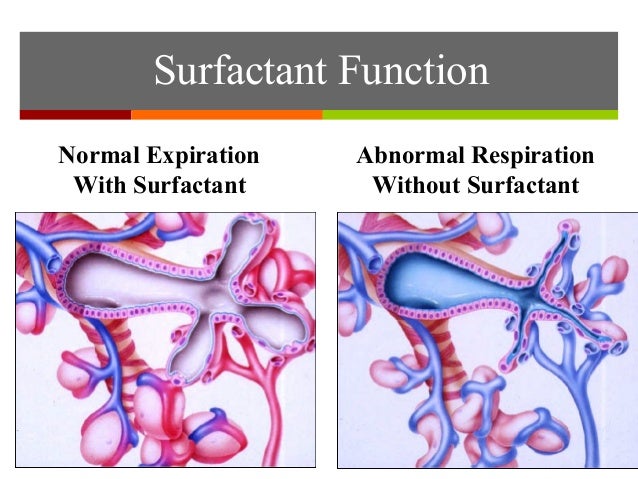
Rds group, with a diagnosis of simple rds (n 80) and rds with pneumonia group, consisting of babies with a diagnosis of rds and a positive balf culture in. Pulmonary surfactant is a mixture of lipids and proteins which is secreted by the epithelial type ii cells into the alveolar space. Synthetic surfactants have been developed and can be used for babies born prematurely (before 34 weeks) who have rds. In addition, they learn how pulmonary surfactant prevents this cohesion, allowing alveoli to. Bleeding into the lungs (pulmonary haemorrhage) occurs mainly in infants born before term (37 weeks� gestation) because of severe lung disease (particularly respiratory distress syndrome, a disease caused by the lack of the normal lining chemicals of the lung (surfactant)) and the need for a breathing machine (assisted ventilation).
 Source:
Source:
Sometimes it is absent in immature lungs and respiratory distress syndrome (rds) can develop. Its main function is to reduce the surface tension at the air/liquid interface in the lung. Synthetic surfactants have been developed and can be used for babies born prematurely (before 34 weeks) who have. The presence of such molecules with surface activity had been suspected since the early 1900s and was finally. Metabolism of surfactant is slower in newborns, especially preterm, than in adults.
 Source: pediatric-neonatalnursingconference.blogspot.com
Source: pediatric-neonatalnursingconference.blogspot.com
If the baby is able to be ventilated at birth, aggressive management can help treat pulmonary hypoplasia (surfactant, nitric oxide treatment up to 40%, high frequency jet or oscillating ventilation, steroids). 24 dying stillborn, 15 dying soon after birth and 16 dying between 2 weeks and 1 year of age with minimal lung pathology. Surfactant replacement therapy for premature babies acts to keep the alveoli from sticking together, and is supplemented with oxygen or ventilation to help the baby breathe. The case allows students to study the microscopic anatomy of lung tissue and come to a deeper understanding of the cohesive property of water that creates surface tension (leading to alveolar collapse) in the underdeveloped lungs of premature babies. Proper lung surfactant is a complex mixture of roughly 90% lipids and 10% proteins in an aqueous.
 Source: holisticdoctoronline.com
Source: holisticdoctoronline.com
Early on, during autopsies, pathologists found stillborn babies’ lungs weirdly inelastic. According to the guardian’s choice, premature infants were grouped into treatment with pulmonary surfactant (ps) combined with nasal continuous positive airway pressure (ncpap; Proper lung surfactant is a complex mixture of roughly 90% lipids and 10% proteins in an aqueous. 24 dying stillborn, 15 dying soon after birth and 16 dying between 2 weeks and 1 year of age with minimal lung pathology. Premature babies around the world are being kept alive thanks to a medical breakthrough that is being trialled.
 Source: nature.com
Source: nature.com
In babies born prematurely, pulmonary surfactant may not be present in adequate amounts _____. When a premature infant whose lungs are not producing enough surfactant is born, those lungs are unable to provide the infant with enough oxygen, which results in respiratory distress syndrome. 34 dying acutely within 2 days of birth from hyaline membrane disease (hmd), 20 dying several days after birth with hmd and its consequences, 8 dying from causes other than hmd; Early on, during autopsies, pathologists found stillborn babies’ lungs weirdly inelastic. Its main function is to reduce the surface tension at the air/liquid interface in the lung.
 Source: highimpact.com
Source: highimpact.com
According to the guardian’s choice, premature infants were grouped into treatment with pulmonary surfactant (ps) combined with nasal continuous positive airway pressure (ncpap; The presence of such molecules with surface activity had been suspected since the early 1900s and was finally. When a premature infant whose lungs are not producing enough surfactant is born, those lungs are unable to provide the infant with enough oxygen, which results in respiratory distress syndrome. 24 dying stillborn, 15 dying soon after birth and 16 dying between 2 weeks and 1 year of age with minimal lung pathology. Surfactant in preterm infants introduction pulmonary surfactant is a complex mixture of phospholipids and proteins that serves to reduce alveolar surface tension.
 Source: slideserve.com
Source: slideserve.com
The observation group) and treatment with ncpap alone (the control group). Preterm infants with respiratory distress syndrome (rds) requiring surfactant therapy have been traditionally receiving surfactant by intubation surfactant and extubation technique (insure), which comprises of tracheal intubation, surfactant administration, and extubation. Lung surfactant was obtained by postmortem lavage from: When a premature infant whose lungs are not producing enough surfactant is born, those lungs are unable to provide the infant with enough oxygen, which results in respiratory distress syndrome. Treatments that specifically target reducing surfactant inactivation would be more effective in adults than replacement lung surfactant therapies that were developed to provide premature babies with lung surfactant.
 Source: slideserve.com
Source: slideserve.com
According to the guardian’s choice, premature infants were grouped into treatment with pulmonary surfactant (ps) combined with nasal continuous positive airway pressure (ncpap; Clements to the field of pulmonary biology stand alone. 24 dying stillborn, 15 dying soon after birth and 16 dying between 2 weeks and 1 year of age with minimal lung pathology. Surfactant replacement therapy for premature babies acts to keep the alveoli from sticking together, and is supplemented with oxygen or ventilation to help the baby breathe. Exogenous surfactant replacement therapy for the treatment of rds in premature infants decreases severe rds, pulmonary air leak syndromes, and death.
 Source:
Source:
Premature babies around the world are being kept alive thanks to a medical breakthrough that is being trialled. A total of 216 premature infants in our hospital were selected. However, more recently noninvasive methods like least invasive surfactant therapy or minimally invasive. Sometimes it is absent in immature lungs and respiratory distress syndrome (rds) can develop. Many babies require respiratory support once they are discharged home.
 Source:
Source:
In pulmonary surfactants, though, there’s a twist, and it would take researchers decades to untangle it. However, more recently noninvasive methods like least invasive surfactant therapy or minimally invasive. If the baby is able to be ventilated at birth, aggressive management can help treat pulmonary hypoplasia (surfactant, nitric oxide treatment up to 40%, high frequency jet or oscillating ventilation, steroids). Rds group, with a diagnosis of simple rds (n 80) and rds with pneumonia group, consisting of babies with a diagnosis of rds and a positive balf culture in. 24 dying stillborn, 15 dying soon after birth and 16 dying between 2 weeks and 1 year of age with minimal lung pathology.
 Source:
Source:
34 dying acutely within 2 days of birth from hyaline membrane disease (hmd), 20 dying several days after birth with hmd and its consequences, 8 dying from causes other than hmd; Surfactant is synthesized, assembled, transported and secreted into the alveolus where it is degraded and then recycled. If the baby is able to be ventilated at birth, aggressive management can help treat pulmonary hypoplasia (surfactant, nitric oxide treatment up to 40%, high frequency jet or oscillating ventilation, steroids). When a premature infant whose lungs are not producing enough surfactant is born, those lungs are unable to provide the infant with enough oxygen, which results in respiratory distress syndrome. Lung scarring sometimes ventilation (begun within 24 hours of birth) or the surfactant used to treat nrds causes scarring to the baby�s lungs, which affects their development.
 Source: slideshare.net
Source: slideshare.net
According to the guardian’s choice, premature infants were grouped into treatment with pulmonary surfactant (ps) combined with nasal continuous positive airway pressure (ncpap; Sometimes it is absent in immature lungs and respiratory distress syndrome (rds) can develop. When a premature infant whose lungs are not producing enough surfactant is born, those lungs are unable to provide the infant with enough oxygen, which results in respiratory distress syndrome. Many babies require respiratory support once they are discharged home. 1 systematic reviews of randomized, controlled trials confirmed that surfactant administration in preterm infants with established respiratory distress syndrome (rds) reduces mortality, decreases the incidence of pulmonary air leak (pneumothoraces and.
Source:
Synthetic surfactants have been developed and can be used for babies born prematurely (before 34 weeks) who have. Lung surfactant was obtained by postmortem lavage from: Bleeding into the lungs (pulmonary haemorrhage) occurs mainly in infants born before term (37 weeks� gestation) because of severe lung disease (particularly respiratory distress syndrome, a disease caused by the lack of the normal lining chemicals of the lung (surfactant)) and the need for a breathing machine (assisted ventilation). Premature babies around the world are being kept alive thanks to a medical breakthrough that is being trialled. 34 dying acutely within 2 days of birth from hyaline membrane disease (hmd), 20 dying several days after birth with hmd and its consequences, 8 dying from causes other than hmd;
 Source: bbc.co.uk
Source: bbc.co.uk
The observation group) and treatment with ncpap alone (the control group). The case allows students to study the microscopic anatomy of lung tissue and come to a deeper understanding of the cohesive property of water that creates surface tension (leading to alveolar collapse) in the underdeveloped lungs of premature babies. According to the guardian’s choice, premature infants were grouped into treatment with pulmonary surfactant (ps) combined with nasal continuous positive airway pressure (ncpap; The presence of such molecules with surface activity had been suspected since the early 1900s and was finally. If the baby is able to be ventilated at birth, aggressive management can help treat pulmonary hypoplasia (surfactant, nitric oxide treatment up to 40%, high frequency jet or oscillating ventilation, steroids).
 Source: researchgate.net
Source: researchgate.net
Defective pulmonary surfactant metabolism results in respiratory distress with attendant morbidity and mortality. Surfactant is synthesized, assembled, transported and secreted into the alveolus where it is degraded and then recycled. The observation group) and treatment with ncpap alone (the control group). Many babies require respiratory support once they are discharged home. 24 dying stillborn, 15 dying soon after birth and 16 dying between 2 weeks and 1 year of age with minimal lung pathology.
 Source: breathe.ersjournals.com
Source: breathe.ersjournals.com
Rds group, with a diagnosis of simple rds (n 80) and rds with pneumonia group, consisting of babies with a diagnosis of rds and a positive balf culture in. Bleeding into the lungs (pulmonary haemorrhage) occurs mainly in infants born before term (37 weeks� gestation) because of severe lung disease (particularly respiratory distress syndrome, a disease caused by the lack of the normal lining chemicals of the lung (surfactant)) and the need for a breathing machine (assisted ventilation). When a premature infant whose lungs are not producing enough surfactant is born, those lungs are unable to provide the infant with enough oxygen, which results in respiratory distress syndrome. Proper lung surfactant is a complex mixture of roughly 90% lipids and 10% proteins in an aqueous. Rds group, with a diagnosis of simple rds (n 80) and rds with pneumonia group, consisting of babies with a diagnosis of rds and a positive balf culture in.
 Source: holisticdoctoronline.com
Source: holisticdoctoronline.com
Pulmonary surfactant is a mixture of lipids and proteins which is secreted by the epithelial type ii cells into the alveolar space. Steroids work best when they are given between 24 hours and 7 days before birth, so theyre not useful in every pregnancy. Lung scarring sometimes ventilation (begun within 24 hours of birth) or the surfactant used to treat nrds causes scarring to the baby�s lungs, which affects their development. 34 dying acutely within 2 days of birth from hyaline membrane disease (hmd), 20 dying several days after birth with hmd and its consequences, 8 dying from causes other than hmd; Synthetic surfactants have been developed and can be used for babies born prematurely (before 34 weeks) who have.
This site is an open community for users to do submittion their favorite wallpapers on the internet, all images or pictures in this website are for personal wallpaper use only, it is stricly prohibited to use this wallpaper for commercial purposes, if you are the author and find this image is shared without your permission, please kindly raise a DMCA report to Us.
If you find this site value, please support us by sharing this posts to your preference social media accounts like Facebook, Instagram and so on or you can also save this blog page with the title pulmonary surfactant in premature babies by using Ctrl + D for devices a laptop with a Windows operating system or Command + D for laptops with an Apple operating system. If you use a smartphone, you can also use the drawer menu of the browser you are using. Whether it’s a Windows, Mac, iOS or Android operating system, you will still be able to bookmark this website.
