Surfactant use in premature babies information
Home » Trend » Surfactant use in premature babies informationYour Surfactant use in premature babies images are available. Surfactant use in premature babies are a topic that is being searched for and liked by netizens today. You can Find and Download the Surfactant use in premature babies files here. Get all royalty-free vectors.
If you’re looking for surfactant use in premature babies pictures information linked to the surfactant use in premature babies interest, you have visit the ideal site. Our site frequently provides you with suggestions for downloading the highest quality video and picture content, please kindly surf and locate more informative video content and graphics that fit your interests.
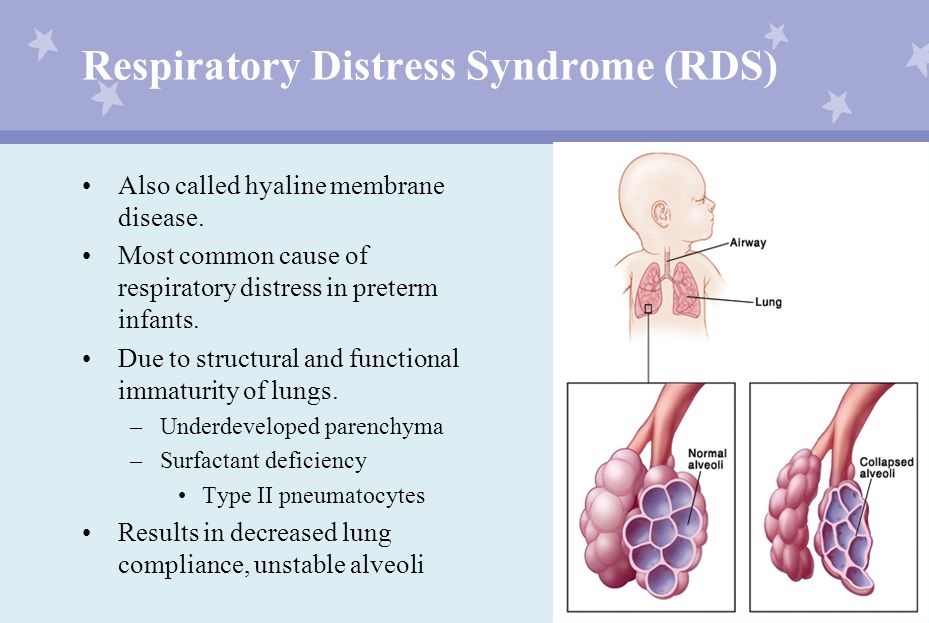
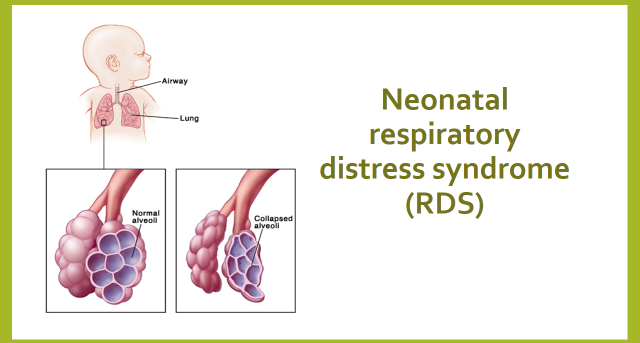
Surfactant Use In Premature Babies. Premature babies often require a surfactant injection to help their lungs to work. A total of 216 premature infants in our hospital were selected. Summary pulmonary surfactant is a complex mixture of specific lipids, proteins and carbohydrates, which is produced in the lungs by type ii alveolar epithelial cells. 1 in preparation for breathing air, fetuses begin producing surfactant during the third trimester of.
 A recent medical technique, known as Less invasive From vajiramias.com
A recent medical technique, known as Less invasive From vajiramias.com
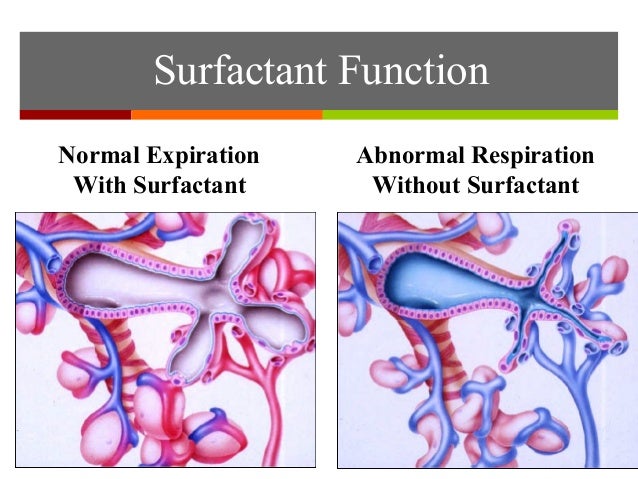
1 systematic reviews of randomized, controlled trials confirmed that surfactant administration in preterm infants with established respiratory distress syndrome (rds) reduces mortality, decreases the incidence of pulmonary air leak (pneumothoraces and. To reduce the risk of lung injury in premature babies, healthcare providers now prefer to use breathing machines that don’t enter the windpipe but use a mask and continuous positive airway pressure (cpap) instead (figure 1). Surfactant replacement therapy for premature babies acts to keep the alveoli from sticking together, and is supplemented with oxygen or ventilation to help the baby breathe. Surfactant in preterm infants introduction pulmonary surfactant is a complex mixture of phospholipids and proteins that serves to reduce alveolar surface tension. A systematic review and meta. Less invasive surfactant administration versus intubation for surfactant delivery in preterm infants with respiratory distress syndrome:
Lung scarring sometimes ventilation (begun within 24 hours of birth) or the surfactant used to treat nrds causes scarring to the baby�s lungs, which affects their development.
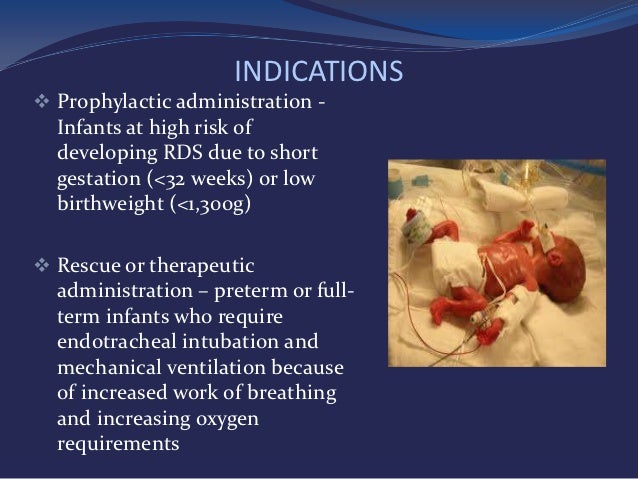
Neonates at risk of developing rds (e.g. The presence of such molecules with surface activity had been suspected since the early 1900s and was finally. Neonates at risk of developing rds (e.g. The history of rds research is a splendid example of how. Rds group, with a diagnosis of simple rds (n 80) and rds with pneumonia group, consisting of babies with a diagnosis of rds and a positive balf culture in. The lungs of premature infants, however, have not developed enough alveoli or type ii alveolar cells to produce the amount of surfactant needed to breathe properly.
Source:
Natural surfactant is produced by the fetus before they are born and their lungs are prepared to breathe properly by about 37 week gestation. Surfactant replacement therapy for premature babies acts to keep the alveoli from sticking together, and is supplemented with oxygen or ventilation to help the baby breathe. 1 systematic reviews of randomized, controlled trials confirmed that surfactant administration in preterm infants with established respiratory distress syndrome (rds) reduces mortality, decreases the incidence of pulmonary air leak (pneumothoraces and. The respiratory distress syndrome (rds) is a lung disorder that is mostly seen in preterm babies, especially those born before week 30. It is caused by a lack of surfactant, which is a substance that coats the inside of the lungs and prevents the small air sacs (alveoli) from collapsing.
 Source: vajiramias.com
Source: vajiramias.com
The lungs of premature infants, however, have not developed enough alveoli or type ii alveolar cells to produce the amount of surfactant needed to breathe properly. They have mainly used single doses varying from 25 mg to 200 mg. Why is surfactant given to premature babies.the surfactant mixture is an essential group of molecules to support air breathing. 1 systematic reviews of randomized, controlled trials confirmed that surfactant administration in preterm infants with established respiratory distress syndrome (rds) reduces mortality, decreases the incidence of pulmonary air leak (pneumothoraces and. The lungs of premature infants, however, have not developed enough alveoli or type ii alveolar cells to produce the amount of surfactant needed to breathe properly.
 Source: paediatricfoam.com
Source: paediatricfoam.com
Physicians use two strategies for administering surfactant. Physicians use two strategies for administering surfactant. Surfactant replacement therapy for premature babies acts to keep the alveoli from sticking together, and is supplemented with oxygen or ventilation to help the baby breathe. Some are from animal lungs or human amniotic fluid, some are synthetic. Premature babies often require a surfactant injection to help their lungs to work.
 Source:
Source:
Surfactant replacement therapy should be considered in: They have mainly used single doses varying from 25 mg to 200 mg. They have been given either at birth as a prophylaxis for neonatal respiratory distress syndrome or as rescue treatment for babies in respiratory failure. Today, rds is an uncommon cause of neonatal mortality in developed nations because it can be successfully treated. A systematic review and meta.
 Source: youtube.com
Source: youtube.com
Additionally, the high cost and complex production of animal surfactant have led to the testing of synthetic Surfactant in preterm infants introduction pulmonary surfactant is a complex mixture of phospholipids and proteins that serves to reduce alveolar surface tension. The observation group) and treatment with ncpap alone (the control group). Some are from animal lungs or human amniotic fluid, some are synthetic. Natural surfactant is produced by the fetus before they are born and their lungs are prepared to breathe properly by about 37 week gestation.
 Source:
Source:
Surfactant replacement therapy for premature babies acts to keep the alveoli from sticking together, and is supplemented with oxygen or ventilation to help the baby breathe. It is caused by a lack of surfactant, which is a substance that coats the inside of the lungs and prevents the small air sacs (alveoli) from collapsing. Why is surfactant given to premature babies.the surfactant mixture is an essential group of molecules to support air breathing. The presence of such molecules with surface activity had been suspected since the early 1900s and was finally. Neonates at risk of developing rds (e.g.
 Source: slideserve.com
Source: slideserve.com
1 in preparation for breathing air, fetuses begin producing surfactant during the third trimester of. The lungs of premature infants, however, have not developed enough alveoli or type ii alveolar cells to produce the amount of surfactant needed to breathe properly. Premature babies around the world are being kept alive thanks to a medical breakthrough that is being trialled. 1 systematic reviews of randomized, controlled trials confirmed that surfactant administration in preterm infants with established respiratory distress syndrome (rds) reduces mortality, decreases the incidence of pulmonary air leak (pneumothoraces and. Preterm infants with respiratory distress syndrome (rds) requiring surfactant therapy have been traditionally receiving surfactant by intubation surfactant and extubation technique (insure), which comprises of tracheal intubation, surfactant administration, and extubation.
 Source: newbornsbaby.blogspot.com
Source: newbornsbaby.blogspot.com
According to the guardian’s choice, premature infants were grouped into treatment with pulmonary surfactant (ps) combined with nasal continuous positive airway pressure (ncpap; Neonates at risk of developing rds (e.g. Premature babies often require a surfactant injection to help their lungs to work. It is thawedbeforeusein a dose of 4 ml/kg. The respiratory distress syndrome (rds) is a lung disorder that is mostly seen in preterm babies, especially those born before week 30.
 Source: onlinelibrary.wiley.com
Source: onlinelibrary.wiley.com
According to the guardian’s choice, premature infants were grouped into treatment with pulmonary surfactant (ps) combined with nasal continuous positive airway pressure (ncpap; According to the guardian’s choice, premature infants were grouped into treatment with pulmonary surfactant (ps) combined with nasal continuous positive airway pressure (ncpap; 1 in preparation for breathing air, fetuses begin producing surfactant during the third trimester of. Less invasive surfactant administration versus intubation for surfactant delivery in preterm infants with respiratory distress syndrome: A systematic review and meta.
 Source: bbc.co.uk
Source: bbc.co.uk
Lung scarring sometimes ventilation (begun within 24 hours of birth) or the surfactant used to treat nrds causes scarring to the baby�s lungs, which affects their development. However, more recently noninvasive methods like least invasive surfactant therapy or minimally invasive. Several clinical reports have shown that intratracheal instillation of large doses of … Premature babies often require a surfactant injection to help their lungs to work. The observation group) and treatment with ncpap alone (the control group).
 Source:
Source:
Search for more papers by this author. 1 systematic reviews of randomized, controlled trials confirmed that surfactant administration in preterm infants with established respiratory distress syndrome (rds) reduces mortality, decreases the incidence of pulmonary air leak (pneumothoraces and. Department of pediatrics, ovum woman and child speciality hospital, bangalore, india. Natural surfactant is produced by the fetus before they are born and their lungs are prepared to breathe properly by about 37 week gestation. A systematic review and meta.
 Source: verywellhealth.com
Source: verywellhealth.com
The lungs of premature infants, however, have not developed enough alveoli or type ii alveolar cells to produce the amount of surfactant needed to breathe properly. However, more recently noninvasive methods like least invasive surfactant therapy or minimally invasive. <32 weeks or low birth weight <1300g) neonates who are intubated, regardless of gestation, and requiring fio 2 >40%. Abhishek somasekhara aradhya md, dm. The presence of such molecules with surface activity had been suspected since the early 1900s and was finally.
 Source: rum.bodrumairport.org
Source: rum.bodrumairport.org
Rds group, with a diagnosis of simple rds (n 80) and rds with pneumonia group, consisting of babies with a diagnosis of rds and a positive balf culture in. The review of trials found evidence that synthetic surfactant for babies with rds is effective. Lung scarring sometimes ventilation (begun within 24 hours of birth) or the surfactant used to treat nrds causes scarring to the baby�s lungs, which affects their development. They have used six surfactant preparations. Several clinical reports have shown that intratracheal instillation of large doses of …
 Source: sec.gov
Source: sec.gov
They have mainly used single doses varying from 25 mg to 200 mg. They have mainly used single doses varying from 25 mg to 200 mg. Department of pediatrics, ovum woman and child speciality hospital, bangalore, india. The history of rds research is a splendid example of how. They have been given either at birth as a prophylaxis for neonatal respiratory distress syndrome or as rescue treatment for babies in respiratory failure.
 Source: mprnews.org
Source: mprnews.org
Neonates at risk of developing rds (e.g. A total of 216 premature infants in our hospital were selected. Surfactant replacement therapy for premature babies acts to keep the alveoli from sticking together, and is supplemented with oxygen or ventilation to help the baby breathe. Premature babies around the world are being kept alive thanks to a medical breakthrough that is being trialled. First, using a preventative strategy, physicians administer artificial surfactant to premature infants who are at risk for developing respiratory distress.
 Source: slideshare.net
Source: slideshare.net
However, more recently noninvasive methods like least invasive surfactant therapy or minimally invasive. It is thawedbeforeusein a dose of 4 ml/kg. Additionally, the high cost and complex production of animal surfactant have led to the testing of synthetic The presence of such molecules with surface activity had been suspected since the early 1900s and was finally. The observation group) and treatment with ncpap alone (the control group).
 Source: researchgate.net
Source: researchgate.net
First, using a preventative strategy, physicians administer artificial surfactant to premature infants who are at risk for developing respiratory distress. According to the guardian’s choice, premature infants were grouped into treatment with pulmonary surfactant (ps) combined with nasal continuous positive airway pressure (ncpap; Some are from animal lungs or human amniotic fluid, some are synthetic. They have mainly used single doses varying from 25 mg to 200 mg. It is thawedbeforeusein a dose of 4 ml/kg.
This site is an open community for users to do submittion their favorite wallpapers on the internet, all images or pictures in this website are for personal wallpaper use only, it is stricly prohibited to use this wallpaper for commercial purposes, if you are the author and find this image is shared without your permission, please kindly raise a DMCA report to Us.
If you find this site convienient, please support us by sharing this posts to your favorite social media accounts like Facebook, Instagram and so on or you can also bookmark this blog page with the title surfactant use in premature babies by using Ctrl + D for devices a laptop with a Windows operating system or Command + D for laptops with an Apple operating system. If you use a smartphone, you can also use the drawer menu of the browser you are using. Whether it’s a Windows, Mac, iOS or Android operating system, you will still be able to bookmark this website.
